The WHO has declared monkeypox a public health emergency of international concern. A case of monkeypox has now been reported in Delhi that does not have an international travel history.
Is it a community spread? How can you protect yourself from this infectious disease?
ORIGIN
Monkeypox is not a novel disease. It was first isolated in the late 1950s from a colony of monkeys. The virus is in the same genus as variola (causative agent of smallpox) and vaccinia viruses (the virus used in one of the available smallpox vaccines). It gets its name from a 1958 outbreak among a group of laboratory test monkeys inside a research facility in Copenhagen, Denmark.
ZOONOTIC DISEASE – HOW DOES IT SP?
“There is a significant role of animals in the spread of monkeypox. Man and monkeys are both accidental hosts and wild rodents are usually seen harbouring this virus. The strain isolated from West Africa appears to be less virulent than the one from Central Africa. It’s clad 2 i.e. West African strain is spreading all over world,” said Dr Dhiren Gupta, Intensivist and Senior Consultant at Sir Gangaram Hospital.
Prolonged contact with animals (monkeys, squirrels, wild rodents) or animal meat (wild animals) or close contact with infected persons. Primarily, it doesn’t spread via air but if someone is in close contact with the infected patient (> 3 hours, within 2 meters) can get infection via large droplets. Secondary attack rates are around 7 percent. It’s less infective than smallpox and chickenpox.
WHO IS AT HIGH RISK OF CONTACTING MONKEYPOX?
Men – Most cases of monkeypox have been seen in men.
LGBTQ – Men who have sex with men and the LGBTQ community have been flagged by the WHO.
Healthcare workers – Prolonged and close exposure to treating the patient could lead to spread through droplets to skin contact as well.
Immunocompromised people – People with prolonged health complications
IT IS A SEXUALLY TRANSMITTED DISEASE (STD) ONLY?
The WHO pointed out, “For the moment this is an outbreak that is concentrated among men who have sex with men, especially those with multiple sexual partners.” Dr Tedros added, “It’s therefore essential that all countries work closely with communities of men who have sex with men, to design & deliver effective information & services, and to adopt measures that protect both the health, human rights & dignity of affected communities.”
But is it an STD? Health experts and epidemiologists disagree. “We have not generated evidence to say that it is only an STD, or spreads through the sexually transmitted disease modes of sexual contact only. It is not like HIV, we can’t categorise it explicitly as HIV only, but these men are in close contact with each other. There are other modes of spread, such as unsafe and unchecked blood transfusions also,” said Dr Sanjay Rai, Professor, Community Medicine AIIMS. Dr Rai is also a national trainer on HIV / AIDS Counselling and Sexually Transmitted Infection (STI) for NACO, Ministry of Health and Family Welfare, Govt. of India, since 1997 and 2008.
“The categorisation of patients of high risk status has been given to men who have sex with men. But that is not the case. Anyone can get monkeypox if they come in contact with those who have these skin regions up until scabs are formed and a normal skin comes back,” said Dr Giridhar Babu, Professor and Head Life Course Epidemiology at Public Health Foundation of India.
Dr Gupta explains the stages of symptoms
Prodromal phase – typically lasts up to five days, is characterised by fever, intense headache, lymphadenopathy, back pain, myalgia, and severe fatigue. Swelling of the lymph nodes may be generalised (involving many different locations on the body) or localised to several areas.
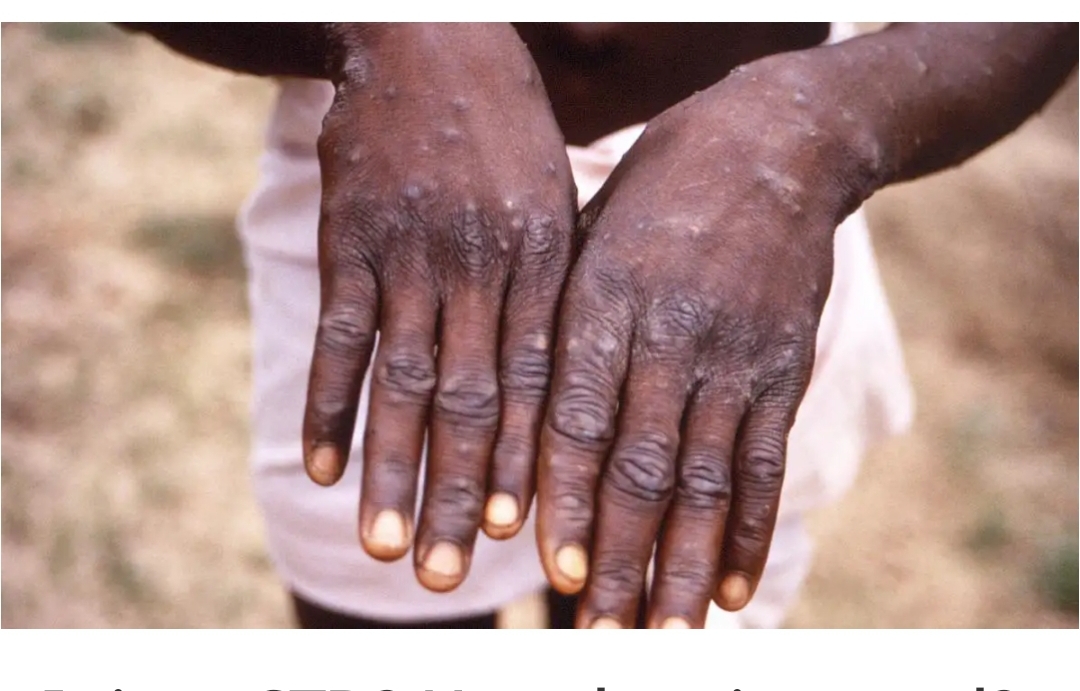
Rash – The skin eruption usually begins within one to four days of appearance of fever and continues for a period of two to three weeks, although rashes without a prodrome have been reported. Rash is painful to start with but becomes itchy. The rash typically begins as 2 to 5 mm diameter macules. Macules subsequently evolve to papules, vesicles, and then pustules.
Lesions are well circumscribed, deep seated, and often develop umbilication (a central depression on the top of the lesion), this could begin from the face, then go to the palm of the hands and soles of the feet.
Multiple nonspecific laboratory findings can be seen in patients with monkeypox. These include abnormal aminotransferases, leukocytosis, thrombocytopenia, and hypoalbuminemia.
WHAT TO DO WHEN YOU COME IN CONTACT WITH MONKEYPOX?
” A smallpox vaccination, if given within 4 days, can prevent disease. Although vaccination can be considered for up to 14 days of exposure, if given between days 4 and 14, vaccination is thought to reduce the symptoms of disease but NOT prevent the disease,” said Dr Gupta.
Indicated treatment suggests – Those with severe disease and those at risk for severe disease (eg, those younger than 8 years of age, pregnant or breastfeeding women, patients with complications of the infection, immunocompromised patients). “At this time, tecovirimat is the treatment of choice, although some experts may suggest dual therapy with tecovirimat and cidofovir in patients with severe disease,” says Dr Gupta. However, experts also say few people require active intervention through medical treatment in younger people.
HOW CAN YOU PREVENT THE SP?
Isolate yourself to room for three weeks till all lesions scab and fall. Incubation period – The incubation period of monkeypox virus infection is usually from 5 to 13 days but can range from 4 to 21 days.
FASTEST RATE OF SP IN LAST 50 YEARS
Initially this year, 3040 cases of monkeypox had been reported to WHO from 47 countries.
Since then, the outbreak has continued to grow, and there are now more than 16 thousand reported cases from 75 countries and territories, and five deaths, said Dr Tedros. Ever since the first human case was detected in 1970 in Republic of Congo, experts have not seen it spread at a rate in the last 50 years since it was found.
“The first time this disease was reported in human beings in 1970s in the Republic of Congo. There were outbreaks in many African countries. In 2003, an outbreak was seen in the US also. But the transmission of zoonotic diseases has increased in the past few years, whether it is covid19 or any other. We need to conduct further investigations. It could be because animal and human contact has increased, meat consumption of incomplete and uncooked food,” said Dr Sanjay Rai.
“Once it is in the community within a country then the travel history is of no relevance. Traveller history is not an important criteria. There have been guidelines issued by Indian government,” said Dr Giridhar Babu.
VACCINES AGAINST MONKEYPOX
There are two available vaccines that can reduce the risk of developing monkeypox. The modified vaccinia Ankara (MVA) vaccine (JYNNEOS in the United States, IMVANEX in the European Union, and IMVAMUNE in Canada) and ACAM2000 vaccine. “The small pox vaccine only provides 82-85% protection against monkeypox. Even anti viral that has been recommended has no proven efficacy,” said Dr Rai.
“Vaccines are also not free of complications – the vaccines are also known to have serious side effects they are not to be used randomly,” said Dr Babu. India could need to stockpile these vaccines for any impending emergency in the future. “Indian vaccine stockpile for smallpox was abandoned after the eradication of smallpox. We need a renewed focus on having vaccine stocks.” he said.
NO NEED TO PANIC, LOW MORTALITY RATE
“Monkeypox is a self-limiting disease with low mortality. Doesn’t leads to scarring unless immunocompromised, said Dr Gupta, adding, “Those who were born before 1977 likely to have received smallpox vaccination and should offer some protection.”
Dr Rai also points out over the years, the rate of mortality has been low. “A person’s immunity is reduced. 0-10% deaths are reported in the last many years in Africa. Recently, 3% deaths have ben reported in Africa,” he said.
👉 Click here to read the latest Gujarat news on TheLiveAhmedabad.com